TTUHSC Researchers to Study Gene’s Role in Prostate Cancer Metastasis
The American Cancer Society estimates that more than 313,780 cases of prostate cancer will be diagnosed in the United States in 2025, resulting in approximately 35,770 deaths. Bone metastasis — a stage of prostate cancer where the disease spreads to the bones — is the leading cause of prostate cancer-related death and currently remains incurable.
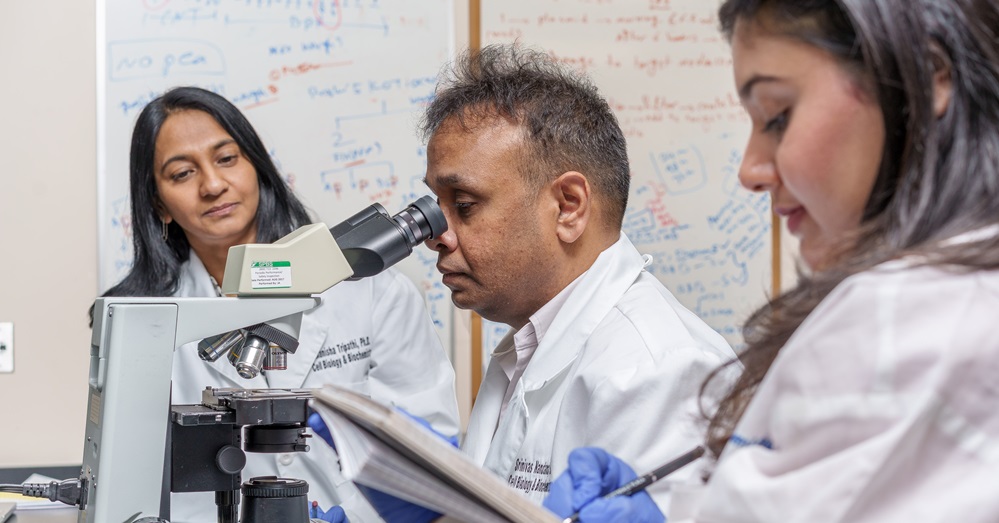
“This stage of prostate cancer is devastating to the patient, as it often affects the bones of the spine, resulting in severe pain from fractures and spinal cord compression, along with significant neurological and functional disabilities,” Srinivas Nandana, Ph.D., said. “The current treatment for this advanced stage of the disease is limited to palliative care aimed at relieving symptoms, with no real hope of reducing or limiting the progression of the disease itself.”
With support from a three-year, $1.85 million grant from the U.S. Department of Defense (DoD) (“Role of TBX2 in the establishment of the Prostate Cancer Pre-Metastatic Niche (PMN) in the Bone”), Nandana and co-investigator Manisha Tripathi, Ph.D., from the Department of Cell Biology and Biochemistry at the Texas Tech University Health Sciences Center (TTUHSC) School of Medicine will investigate the role of TBX2, a transcription factor, in establishing the prostate cancer premetastatic niche in bone. Their research seeks to advance the understanding of prostate cancer metastasis and develop novel treatment strategies.
Nandana’s laboratory has focused on deciphering the role of TBX2 in prostate cancer for more than a decade, supported primarily by grants from the DoD, the Cancer Prevention Research Institute of Texas-Texas Regional Excellence in Cancer, the Ted Nash Long Life Foundation and The CH Foundation. Building on findings from their previous study published in Cancer Research (“Bone Metastasis of Prostate Cancer Can be Therapeutically Targeted at the TBX2-WNT Signaling Axis”) and new data, Nandana and Tripathi will investigate the earliest stages of the bone metastasis process.
During these stages, the primary prostate tumor continually releases tiny sac-like membrane structures called exosomes, which contain proteins and RNA molecules. These exosomes travel through the bloodstream and interact with normal bone cells. Once in the bone, they share their molecular contents, causing the bone cells to “remodel” into a potential future “nesting” site, or “pre-metastatic niche,” making the bone more hospitable to arriving cancer cells.
At some point, Nandana said, a circulating cancer cell homes in on one of these bone nesting sites and then grows, divides and becomes a new metastatic tumor mass.
Nandana said a more complete understanding of this early exosome-mediated communication system between the primary prostate tumor and bone may open up new avenues to intervene and disrupt the process, potentially slowing or even preventing bone metastasis.
In their upcoming studies, Nandana and Tripathi will combine the use of laboratory and mouse models of human prostate cancer with genetic techniques to study the NICD3 protein. Their aim is to determine whether the NICD3 protein, secreted in exosomes due to elevated TBX2 in tumor cells, is essential for creating the bone environment that enables metastatic prostate cancer cells to establish and grow.
“We will also evaluate whether an existing class of anticancer drugs, known as gamma secretase inhibitors (GSIs), can reduce NICD3 formation in primary tumor cells to levels insufficient to initiate the bone remodeling and metastatic process, thereby reducing or potentially preventing prostate cancer bone metastases,” Nandana said. “GSIs are clinically-approved agents, so if successful, direct clinical testing could proceed rapidly.”
If the research proves successful, Nandana said it could lead to new treatment approaches aimed at slowing or preventing prostate cancer bone metastasis, a significant advancement considering that bone metastases are currently incurable and often result in intense pain, fractures and loss of mobility. Stopping metastasis before it begins could significantly improve outcomes and quality of life for patients.
As part of the study, Nandana and Tripathi also will assess drugs already approved for other conditions. If any of these drugs show promise, they could potentially be repurposed for prostate cancer treatment more quickly than newly developed therapies.
“While this research is still in its early stages, it offers promising new insights into how prostate cancer spreads and how we might intervene earlier in that process,” Nandana said. “Bone metastasis causes serious problems for patients, including pain and reduced mobility. If we can better understand how cancer interacts with bone in the early stages, we might be able to reduce the impact of advanced disease. This could help improve comfort and quality of life for some patients, and potentially delay or prevent complications related to bone metastases.”
Related Stories
TTUHSC Cancer Researcher Honored by National Academy of Inventors
C. Patrick Reynolds, M.D., Ph.D., director of the School of Medicine Pediatric Cancer Research Center at TTUHSC, has dedicated his life as a researcher to developing treatments for childhood cancers.
TTUHSC’s Hudson Set to Serve as President for Society of Clinical Research Associates
The Society of Clinical Research Associates (SOCRA) has elected Texas Tech University Health Sciences Center’s (TTUHSC) Catherine Hudson, Dr.P.H., as its president for 2025-2026.
Clinical Research Institute a Source of Pride for Retiring Griswold
Upon his retirement, John Griswold, M.D., reflects on the Clinical Research Institute and what it has achieved.
Recent Stories
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
TTUHSC Receives $1 Million Gift from Amarillo National Bank to Expand and Enhance Pediatric Care in the Panhandle
TTUHSC School of Medicine leaders accepted a $1 million philanthropic gift from Amarillo National Bank on Tuesday (Feb. 10), marking a transformational investment in pediatric care for the Texas Panhandle.
Texas Tech University Health Sciences Center Permian Basin Announces Pediatric Residency Program Gift
TTUHSC Permian Basin, along with the Permian Strategic Partnership and the Scharbauer Foundation, Feb. 5 announced a gift that will fund a new pediatric residency.
