Journal’s Special Edition Recalls Landmark Discovery Made in TTUHSC Lab

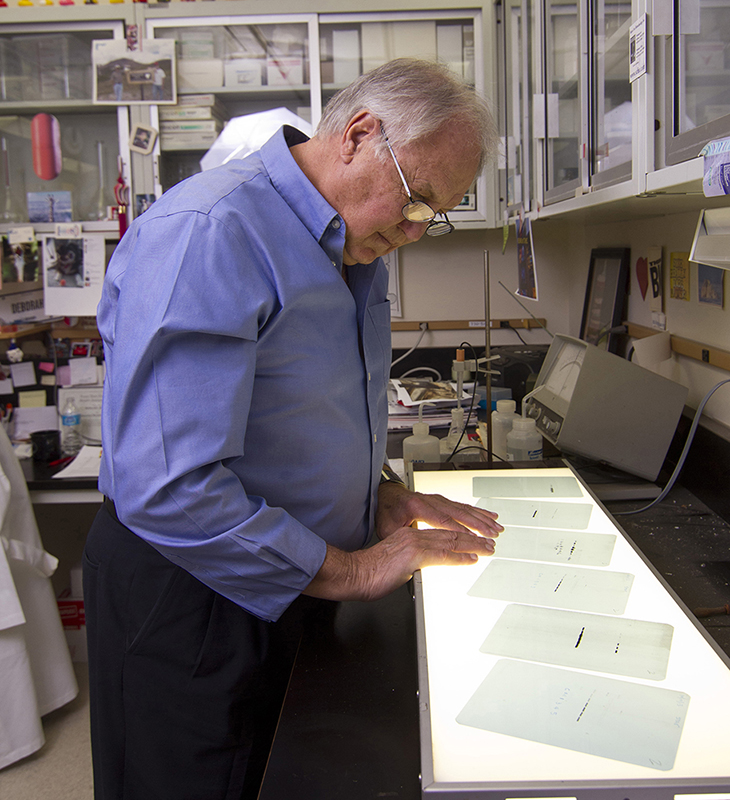
Douglas Stocco, Ph.D.
In September 1994, the Journal of Biological Chemistry published a paper that for the first time described the cloning, sequencing and naming of the Steroidogenic Acute Regulatory (StAR) protein. That paper (“The Purification, Cloning, and Expression of a Novel Luteinizing Hormone-induced Mitochondrial Protein in MA-10 Mouse Leydig Tumor Cells: Characterization of the Steroidogenic Acute Regulatory Protein”) has been cited more than 1,400 times since that initial publication.
The landmark research, conducted at the Texas Tech University Health Sciences Center (TTUHSC) School of Medicine in the Department of Biochemistry laboratory of Douglas Stocco, Ph.D., showed that the StAR protein controls the movement of cholesterol across the mitochondrial membrane, thus regulating steroid biosynthesis in the body. Cholesterol is the precursor of all steroids, and the cholesterol conversion process discovered by Stocco is the first enzymatic step in steroid hormone biosynthesis.
Researching the rapid synthesis of steroid hormones has been the subject of intensive investigation for nearly six decades. These studies have included steroid hormones such as estrogen, progesterone, testosterone, aldosterone and cortisol where synthesis occurs when trophic hormones (e.g., luteinizing hormone and follicle stimulating hormone in reproductive tissues and adrenocorticotropic hormone in the adrenal) interact with the steroidogenic cells in those tissues.
When StAR is expressed in steroidogenic cells, it has been demonstrated that the steroids produced are critical for normal reproductive function and the homeostasis of other bodily functions. Expression of StAR in steroidogenic cells experimentally also can increase steroid production in those cells even in the complete absence of external stimulation.
Further studies have shown that mutations in the StAR gene cause a potentially lethal condition that leads to a total loss of steroid synthesis in afflicted newborns labeled lipoid congenital adrenal hyperplasia (LCAH).
Landmark research, conducted at TTUHSC, has been cited more than 1,400 times since its initial publication.
A key observation made during the 1950s showed that the acute production of steroids required the swift and timely synthesis of new proteins whose role appeared to be involved in the delivery of cholesterol from the outer to the inner mitochondrial membrane where the process of steroidogenesis begins. It was quickly learned that this transfer of cholesterol to the inner membrane was the regulated and rate-limiting step in steroidogenesis. Following this observation, the quest for the putative regulator protein(s) began in earnest in the 1950s and 1960s.
When Stocco arrived at TTUHSC in 1974, he brought with him several projects that were carried over from his postdoctoral years at the University of California, Los Angeles (UCLA). Feeling like he wasn't making much headway with those projects, he decided to turn his investigative focus to identifying the proteins that regulated the movement of cholesterol into the mitochondria.
“The mitochondria are an organelle (specialized structure) inside all cells that produce energy,” Stocco said. “They produce adenosine triphosphate (ATP) in the cells, which is a nucleotide and is the source for energy use and storage and provides animals with the energy to drive and support many processes in living cells.”
While at UCLA, Stocco learned that mitochondria are the location where the first steroid is made. Mitochondria have an inner membrane and an outer membrane. They can convert cholesterol, which is not a steroid, into a compound known as pregnenolone, the first steroid synthesized in steroidogenic cells. Stocco said investigators who performed the early work in the 1950s showed mitochondria were a key to the whole steroid biosynthesis process because mitochondria are where cholesterol is converted into pregnenolone.
“The reason it was so hard to chase that down is because the enzyme to convert cholesterol to pregnenolone is located on the inner side of the inner mitochondrial membrane,” Stocco explained. “That location is usually inaccessible to cholesterol because cholesterol is very hydrophobic, meaning that it hates water, and as such, it cannot traverse through the aqueous areas into the inside of the mitochondria by simple diffusion. Using inhibitors of protein synthesis, several investigators in the 1950s clearly demonstrated that the synthesis of new proteins was an absolute requirement for the cell to produce steroids.”
In the late 1980s, Stocco’s laboratory then began trying to identify the protein(s). Using a steroidogenic cell line (known as a Leydig cell, which can be grown in tissue culture and produces testosterone) and other molecular techniques, they attempted to find and characterize the protein(s).
During the next two decades, several candidate proteins for this function had emerged from other laboratories, which resulted in some controversy in the field. Stocco’s laboratory had observed a series of four mitochondrial proteins and continued to work with them to determine if they were candidates for the elusive regulator.
The purification, cloning and expression of this protein, as published in the 1994 Journal of Biological Chemistry manuscript, demonstrated that the StAR protein met all the criteria for being the true rate-limiting protein. This statement is supported by the fact that StAR appears in steroidogenic cells in a dose responsive, time dependent manner that paralleled the appearance of steroids following the appropriate stimulation.
Furthermore, it was observed that blocking the synthesis of StAR completely inhibited the synthesis of steroid hormones in steroidogenic cells. Also, it was found that genetic mutations in the StAR gene are responsible for causing the potentially lethal LCAH, a condition in which affected children are unable to synthesize steroids of any kind.
Lastly, knockout of the StAR gene in mice eliminated steroid synthesis, a condition similar to LCAH in humans. Stocco noted that most of the credit for establishing the role of StAR in regulating steroidogenesis should be given to Barbara Clark, Ph.D., a former postdoctoral fellow in the Stocco laboratory who took on this difficult project and succeeded in solving the problem admirably.
These findings have transformed the steroid hormone biosynthesis field by solidifying StAR’s vital role in steroid hormone biosynthesis. Scientists also now have a better understanding of other StAR-like proteins that can influence cholesterol transport in both steroidogenic and non-steroidogenic cells, which could lead to potentially targeting StAR and regulating the mitochondria cholesterol levels associated with other disease pathologies such as neuropathies, atherosclerosis and certain liver disease.
Stocco, now a Professor Emeritus at TTUHSC, said a Special Edition for the 30th anniversary of the discovery of StAR will be published by the UK Journal of Endocrinology and Journal of Molecular Endocrinology to highlight the contribution that StAR has made to our understanding of the control of steroid hormone production in steroidogenic cells.
“Thirty years ago, the StAR protein was cloned and sequenced and, when expressed in steroidogenic cells, shown to increase steroid production in the complete absence of external stimulation,” Stocco said. “Shortly thereafter, it was demonstrated that mutations in the StAR gene caused the potentially lethal condition known as lipoid congenital adrenal hyperplasia, which results in the complete loss of steroid synthesis in afflicted newborns. For these reasons, it was concluded that the StAR protein is an indispensable component in steroid hormone biosynthesis, a finding that has solved the mystery of how steroid hormone biosynthesis is regulated.”
Related Stories
National Academy of Inventors Names TTUHSC Faculty Senior Members
The National Academy of Inventors (NAI) has designated two current and one former TTUHSC faculty researchers as Senior Members.
TTUHSC Cancer Researcher Honored by National Academy of Inventors
C. Patrick Reynolds, M.D., Ph.D., director of the School of Medicine Pediatric Cancer Research Center at TTUHSC, has dedicated his life as a researcher to developing treatments for childhood cancers.
TTUHSC’s Hudson Set to Serve as President for Society of Clinical Research Associates
The Society of Clinical Research Associates (SOCRA) has elected Texas Tech University Health Sciences Center’s (TTUHSC) Catherine Hudson, Dr.P.H., as its president for 2025-2026.
Recent Stories
National Academy of Inventors Names TTUHSC Faculty Senior Members
The National Academy of Inventors (NAI) has designated two current and one former TTUHSC faculty researchers as Senior Members.
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
TTUHSC Receives $1 Million Gift from Amarillo National Bank to Expand and Enhance Pediatric Care in the Panhandle
TTUHSC School of Medicine leaders accepted a $1 million philanthropic gift from Amarillo National Bank on Tuesday (Feb. 10), marking a transformational investment in pediatric care for the Texas Panhandle.
