It Takes a Community to Achieve Population-Based Improved Health
A look at the possibilities and benefits of realizing population-based healthcare.

It’s fairly easy to understand primary medical care, the day-to-day medical services that we all require on an individual basis. However, many are not as familiar with the study and practice of population-based healthcare. Population-based healthcare goes beyond granting access to health services. Rather, it focuses on the system established to improve the health outcomes of a group of individuals, allowing communities to give direction to any health initiatives.
We spoke with Debra Flores, Ph.D., Director of the TTUHSC Master of Healthcare Administration Program with the School of Health Professions, and Morgan House, Ph.D., Assistant Professor of the TTUHSC Healthcare Management Program, about the power of population-based healthcare, the obstacles that stand in the way, and what she hopes to see in the future of this vital movement.
What is Population-Based Healthcare?
Drs. Flores and House: Population health has been around for decades. Some define Population health as “health outcomes of a group of individuals including the distribution of such outcomes within the group.” CDC further describes population health as follows: “Population health brings significant health concerns into focus and addresses ways that resources can be allocated to overcome the problems that drive poor health conditions in the population.” To summarize, population health focuses on the health outcomes of the population/community.
How Does Public Health Complement Traditional Clinical Care?

Drs. Flores and House: The traditional role of clinical care is to diagnose and treat patients, including prevention aspects such as immunizations and other health-care screenings. The public health role is to control and prevent diseases in the population. These two practices complement each other and work together for the greater good of the community they serve. This has been very evident during the current pandemic. Public health, clinical care, and acute care have all been working together to address certain aspects of COVID-19 that pertain to their scope of care. During COVID, public health addressed the majority of the screenings, tracking, immunizations, and education. Even though clinical care has done its fair share of immunizations and screenings, its focus is usually on treatment. When individuals’ health becomes too acute to treat in a clinical setting, they are hospitalized. These systems communicated and worked with each other in tandem to improve health outcomes. The pandemic is only one of many examples where public healthcare and traditional healthcare work in unison.
How Has Population-Based Care Evolved?
Drs. Flores and House: Population health became more well-known after the Affordable Care Act was passed in 2010. At this time, the Triple Aim performance framework was introduced, which included:
- Improve the health of populations
- Improve the experience of care
- Reduce health care costs

DSRIP (Delivery System Reform Incentive Payment) and MACRA (Medicaid and CHIP Reauthorization ACT) were introduced in 2015 as value-based care programs. Before DSRIP and MARCA, healthcare providers were paid using a fee-for-service schedule, which meant the more patients one treated, the more one would earn. With this type of health system, healthcare costs increased rapidly and uncontrollably without improving patients’ health outcomes.
According to the Commonwealth Fund, the United States spends more than other countries on health care costs. Given this information, CMS (Centers for Medicaid and Medicare), the most prominent public insurance provider, partnered with private insurance providers to shift from fee-for-service payment schedules toward value-based payment, using the triple-aim model. In this value-based payment model, there is a team effort between insurance providers and health care providers to take responsibility for health outcomes by utilizing resources wisely. This is done through a patient-centered approach. In order to be effective, partnerships must extend to patients, their families, and community organizations.
Even though population-based health care has been around for decades, the delivery was set up for individual care, and a shift needed to take place. Shifting to a population approach expands the reach of care into the community and becomes more of a continuum rather than a straight line.
How Does Community Involvement Factor into Population-Based Care?
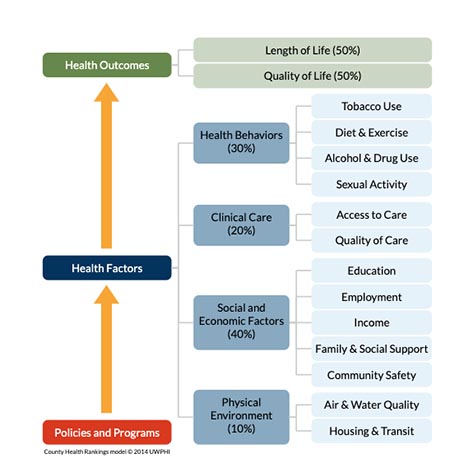
Drs. Flores and House: Community involvement factors into population-based care, and the best way to explain this is by using the County Health Rankings Model. I use this to teach population health, and it is a big eye-opener for many people. It is important to understand that Policies and Programs impact Health Factors and thus Health Outcomes, which highlights the importance of solid policies. The County Health Rankings Model is similar to a logic model starting with Health Outcomes including: Length of Life and Quality of Life. Health Factors and Policies and Programs. (see Figure 1).
Health Factors include the following:
- Health Behaviors (which accounts for 30% of Health Factors)
- Clinical Care (which accounts for 20% of Health Factors)
- Social and Economic Factors (which accounts for 40% of Health Factors)
- Patients' Physical Environment (which accounts for 10% of Health Factors).
Health Behaviors include activities controlled by an individual such as tobacco use, diet and exercise, alcohol and drug use, and sexual activity. Clinical Care includes access and quality of care. Social and Economic Factors include education, employment, income, family and social support, and community safety. The Physical Environment factor includes air and water quality and housing and transportation. Economic and physical environment factors are often not controllable by an individual. These factors have a great impact on an individuals’ health, explaining why health extends far beyond signs and symptoms presented during a clinical or acute medical office visit.
It is most important to note that Clinical Care only accounts for 20% of these factors, with the remainder including: Health Behaviors, Social & Economic Factors, and Physical Environment, accounting for 80 percent of the health factors, thus ultimately impacting overall health outcomes. This finding tells one that a clinical visit can only affect 20 percent of that person’s well-being. The rest is affected by the other factors noted above. Therefore, an individual’s care, treatments and interventions have to extend beyond the clinical visit, beyond the four walls of an office setting, and into the community where individuals live. This continuum of care often includes coordination and programs that offer transitional care.
How Does Population Health Relate to Health Disparities?
Drs. Flores and House: The implementation of population health is not effective unless health disparities are also addressed. Health disparities and social determinants of health are an essential part of an individual's overall health, as demonstrated in the county health rankings graphic.
Another component that affects population health is understanding the difference between equality and equity. The Robert Wood Johnson Foundation has a great illustration of what the difference is between equality and equity. It is not a matter of giving everyone the same care; it is a matter of customizing the care according to individual’s needs. Until this difference is understood and addressed, health outcomes will continue to be negatively affected. Much like Maslow’s Hierarchy of Needs; if an individual does not have food or a safe home to reside in, their focus is not on the medications recently prescribed for a chronic disease but a mere focus on survival.
What are the Obstacles to Population-Based Healthcare?
Drs. Flores and House: Some obstacles to population-based healthcare include: poor coordination and transitions-of -care resulting in inconsistent outcomes, thus leading to higher healthcare costs and lower-quality of care. Resistance from providers to move away from fee-for-service to value-based care was perhaps due to a lack of understanding. Healthcare providers have the patient’s best interest at heart, but were used to the old model of care where the visit ends when the patient walks out of the clinic. However, with that model the vicious cycle that kept patients with chronic conditions coming back with a worsened health status. Individuals are often labeled as non-compliant when the issue is much deeper and broader than non-compliance. Perhaps some of the issues may have been non-compliance, but many of the problems are much deeper than that to include: obtaining and purchasing medication, lack of transportation to get to the health care appointment, access and affordability of fast food, and many other personal barriers. It is difficult and costly to set up a practice to provide coordination and transitional care beyond the four walls of a clinic, so this is one obstacle to population-based health. This is a transition that cannot happen overnight, but it is possible with cost savings such as: bundled payments, patient-centered medical home models, and value-based purchasing initiatives just to name a few.
What Do You See in the Future of Population-Based Healthcare?
Drs. Flores and House: More patient-centered medical home models implemented in private practices where care extends to the community would be optimal. Our healthcare system was on a track toward this model of care when the pandemic hit, which created further obstacles and barriers including healthcare personnel shortages. During this pandemic, attitudes and differences toward a one-team healthcare approach have shifted. This can be viewed as either positive or negative, depending on which side of the fence one stands. Although much work needs to be carried out, coordinated efforts created during the pandemic can be utilized moving forward. It is vital to break down the silos, involve communities, knowing the difference between equity and equality, and quality versus quantity.
Related Stories
TTUHSC Receives $1 Million Gift from Amarillo National Bank to Expand and Enhance Pediatric Care in the Panhandle
TTUHSC School of Medicine leaders accepted a $1 million philanthropic gift from Amarillo National Bank on Tuesday (Feb. 10), marking a transformational investment in pediatric care for the Texas Panhandle.
Texas Tech University Health Sciences Center Permian Basin Announces Pediatric Residency Program Gift
TTUHSC Permian Basin, along with the Permian Strategic Partnership and the Scharbauer Foundation, Feb. 5 announced a gift that will fund a new pediatric residency.
The Ph.D. Programs that Shape Health Care
The Graduate School of Biomedical Sciences Ph.D. programs at TTUHSC provide the foundation, mentorship and research opportunities you need to pursue groundbreaking work.
Recent Stories
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
TTUHSC Receives $1 Million Gift from Amarillo National Bank to Expand and Enhance Pediatric Care in the Panhandle
TTUHSC School of Medicine leaders accepted a $1 million philanthropic gift from Amarillo National Bank on Tuesday (Feb. 10), marking a transformational investment in pediatric care for the Texas Panhandle.
Texas Tech University Health Sciences Center Permian Basin Announces Pediatric Residency Program Gift
TTUHSC Permian Basin, along with the Permian Strategic Partnership and the Scharbauer Foundation, Feb. 5 announced a gift that will fund a new pediatric residency.
