Waging Battle Against Opioid Crisis
TTUHSC Making Impact in Research, Outreach Efforts
Original story found on https://yourlifeourpurpose.org/stories/ttuhsc-opioid-research.aspx
More than two million Americans struggle with opioid use disorders, and 130 people
die every day from opioid overdose — a statistic rivaling some of the more common
major diseases —causing most experts to declare a nationwide opioid epidemic.
Texas Tech University Health Sciences Center researchers in the Department of Pharmacology
and Neurosciences are currently conducting studies to understand the devastating hold
of these drugs and develop new therapies to fight the opioid crisis.
Josée Guindon, Ph.D., DVM, assistant professor, brings her experiences with veterinary medicine together with her interest in pain management to find solutions for addiction to opioids.
“There’s the possibility of creating different compounds to get the analgesic effect without the other side effects like addiction,” she said. “There’s also the option to combine a lower dose of cannabinoids with opioids and see if we can get the beneficial effects of both of them without developing dependency and addiction.”
Guindon said that there are multiple levels of pain, which is why she believes multidisciplinary approaches are key to pain management.
Sensory: stumping your toe — feeling pain from the hurt.
Cognitive: Thought process associated with the injury: “Will this force me to take time off
work? What about my finances? Will I be able to walk normally after the injury?”
Emotional: “How will this affect my work, my ability to take care of my family? What will I
be able to do, what will I have to give up? How will I feel about this injury and
loss of function?”
“If you’re in chronic pain for months because of a surgery or broken bone, your emotional stability is affected,” she said. “However, the doctor has prescribed you with an opioid for the sensory level of your pain, causing you to forget about your cognitive and emotional difficulties associated with that pain. Therefore, you have an increased risk of dependency on these drugs if the sensory component of pain is the only thing addressed by your physician.”
Guindon’s colleague, Khalid Benamar, Ph.D., associate professor, is working in two areas of opioid-related research. His research focuses on reduced responsiveness to opioids and brain abnormalities resulting from chronic use of drugs as underlying causes of opioid dependence and addiction.
In April 2018, the National Institutes of Health launched the HEAL (Helping to End Addiction Long-term) Initiativeto address the national opioid public health crisis. Opioids are powerful pain relievers but can lose effectiveness over time and have severe side effects, including the risk of addiction and increased sensitivity to pain, said Volker Neugebauer, Ph.D., chair of the Department of Pharmacology and Neurosciences and Giles C. McCrary Endowed Chair in Addiction Medicine.
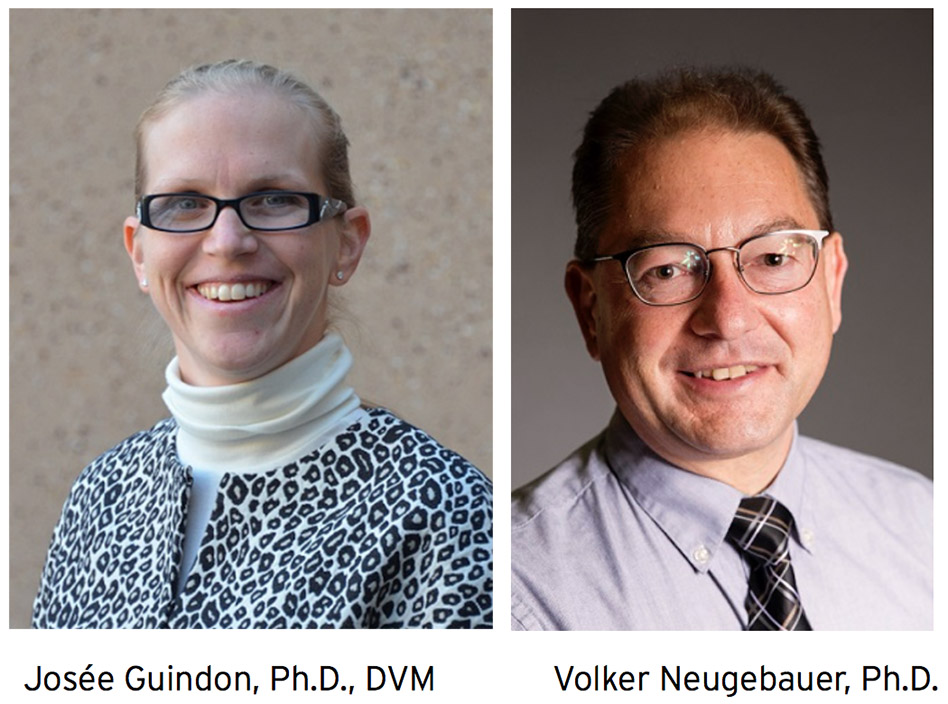
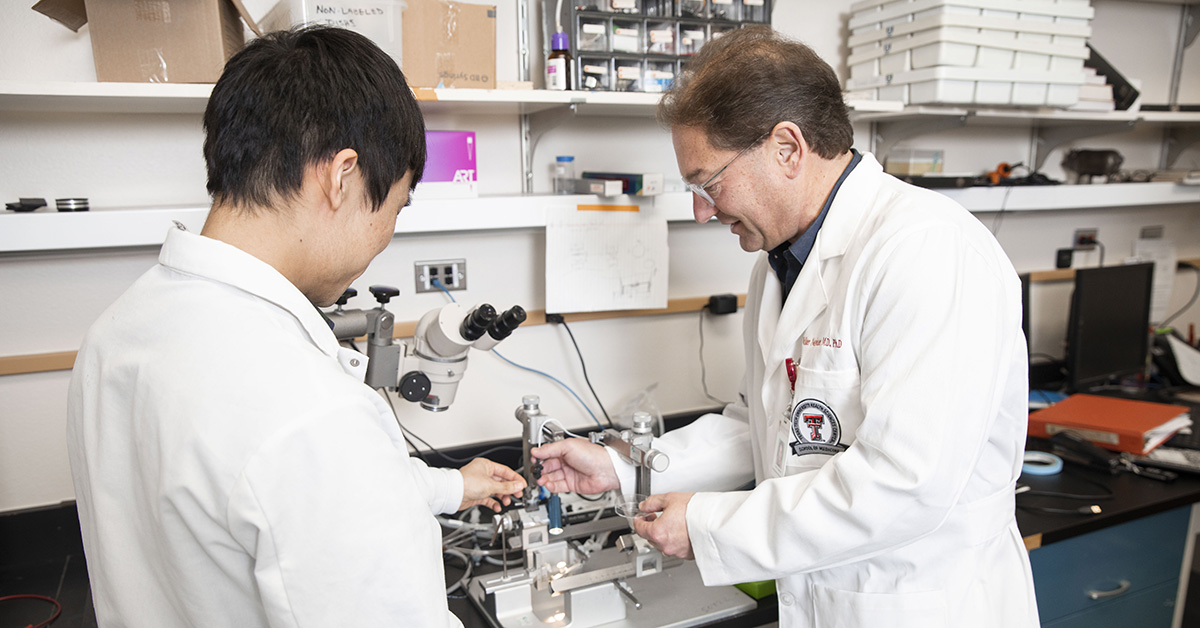
At the time the HEAL Initiative was launched, Neugebauer's research group was awarded a collaborative $2.7 million NIH grant, working together with colleagues at the University of Arizona (Frank Porreca, Ph.D., and Edita Navratilova, Ph.D.) Opioid analgesia and addiction involve mechanisms of action in brain areas that affect what Neugebauer's group has been studying for two decades: The amygdala, a key player in emotions, particularly negative emotions such as fear and anxiety, is part of the limbic system which is concerned with learning and memory, emotional regulation, drives and reward.
Their study tests the novel hypothesis that blocking a specific target of opioids (so-called kappa opioid receptors) in the brain (amygdala) provides pain relief without side effects or addiction in chronic pain. In contrast, current opioid medications activate specific opioid receptors, which can lead to tolerance and even increased pain sensitivity.
Neugebauer and Guangchen Ji, Ph.D., research associate professor, along with Nadia German, Ph.D., assistant professor, and Anwar Hossain, MPHarm, colleagues at in the School of Pharmacy at Amarillo, have filed a provisional patent application for this novel compound to block kappa opioid receptors, which was discovered and developed by German's team.
“One thing we know for sure,” Guindon said, “is the more we know, the more we realize how much we don’t know. Our knowledge is continually increasing, and pain management is constantly evolving — we just recently started studying sex differences and how men and women differ in their responses to pain — so I think the work we are doing will certainly impact this crisis for the better.”
“Technically this isn’t a new problem,” said Zach Sneed, Ph.D., CRC, LCDC, program director for the Master of Science in Addiction Counseling in the School of Health Professions Department of Clinical Counseling and Mental Health. “What is new, is the expansion of the menu, so-to-speak. We have more options today in our choice of opioids. Whereas the epidemics of the 1960s and 1980s were focused on heroin, this current epidemic is different because of the huge influx of prescription opioids, as well as synthetic opioids like fentanyl and carfentanil. There are more choices available than we’ve ever seen before.”
The question for most health care professionals is, how did this epidemic happen?
According to the National Institutes of Health (NIH) National Institute on Drug Abuse (NIDA), starting in the late 1990s, pharmaceutical companies reassured the medical community that patients would not become addicted to prescription opioid pain relievers. Health care providers began prescribing them at higher rates, subsequently leading to a widespread diversion and misuse of these medications before it became clear that the opioids were at fault.
Effective Treatment on the Street
The U.S. Department of Health and Human Services is focusing its efforts on five major priorities in addressing the opioid epidemic, according to the NIDA website. The first one is improving access to treatment and recovery services. At the National RX Drug Abuse and Heroin Summit in 2017, Thomas E. Price, M.D., said 90 percent of Americans struggling with addiction are not currently getting treatment.
“There are a couple of different treatment models for opioid use disorder,” Sneed said. “The one that is considered the ‘gold standard’ of treatment is medication-assisted treatment or MAT as it’s often referred to. We say this is the gold standard because it allows that client or patient or person with the disorder to interact with a care team.”
This team of professionals could involve physicians, nurses, counselors, etc., all working to find long-term solutions for people with this disorder. The medication used for treatment is either an agonist or antagonist, said Sneed, and it blocks the effects of other opioids. Another version can partially activate the opioid receptors, so the person doesn’t experience any craving. The individual seeking treatment is prescribed medication, which paired with counseling and therapy, helps them build new skills and learn how to deal with some of the things that medicine may not help with such as psychological issues.
One medication that can stop a fatal overdose from happening is Naloxone, also known as Narcan. The drug reverses the effects of an opioid overdose within seconds, according to Jason Cooper, PA-C, who serves as director of TTUHSC Special Medical Operations and as medical director for the Midland Police Department.
Through Cooper’s efforts, each police officer in Midland carries a Narcan kit. Since adding the protocol to the department in May, the officers have administered the drug three times for overdoses, according to the Midland Police Department. “They’re (police officers) the first ones on the scene most of the time — first ones called to check on suspicious activity or make welfare checks,” Cooper said.
“Since Narcan blocks the effects almost immediately; our first responders have the
opportunity to save lives they didn’t have before.”
The “kit” is a pre-packaged syringe accompanied by a device engineered to administer
the medication through the nasal route. Cooper said there are no needles involved
to minimize the risk of exposure to bloodborne pathogens. Instead, the officer sprays
it in the person’s nose, and the drug is absorbed directly into the bloodstream through
the nasal membranes.
“The nose is highly vascular, so the absorption of medications is very effective,” Cooper added.
TTUHSC faculty feel a responsibility to provide for community needs because they’re proud to serve as a health resource for all people in West Texas and beyond.
“One of our duties as a health sciences center is to go out and provide care and promote education and even serve in nontraditional capacities,” said Cooper. “The traditional things are people go to our medical school, they go to our classes, they go to our programs, but the nontraditional things involve being a health resource outside of our classrooms. We have the expertise to share outside of our buildings, too — we should be looking for ways to engage our communities in which we have a presence — and we should be looking to offer technical assistance or oversee programs that promote public safety.”
Related Stories
Celebrating Veterans: TTUHSC’s General Martin Clay’s Legacy of Service and Leadership
From his initial enlistment in the Army National Guard 36 years ago to his leadership in military and civilian health care management roles, Major General Martin Clay’s career has been shaped by adaptability, mission focus and service to others.
Texas Tech University Health Sciences Center School of Nursing Named Best Accelerated Bachelor of Science in Nursing Program in Texas
The TTUHSC School of Nursing Accelerated Bachelor of Science in Nursing (BSN) program has been ranked the No. 1 accelerated nursing program in Texas by RegisteredNursing.org.
TTUHSC Names New Regional Dean for the School of Nursing
Louise Rice, DNP, RN, has been named regional dean of the TTUHSC School of Nursing on the Amarillo campus.
Recent Stories
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
TTUHSC Receives $1 Million Gift from Amarillo National Bank to Expand and Enhance Pediatric Care in the Panhandle
TTUHSC School of Medicine leaders accepted a $1 million philanthropic gift from Amarillo National Bank on Tuesday (Feb. 10), marking a transformational investment in pediatric care for the Texas Panhandle.
Texas Tech University Health Sciences Center Permian Basin Announces Pediatric Residency Program Gift
TTUHSC Permian Basin, along with the Permian Strategic Partnership and the Scharbauer Foundation, Feb. 5 announced a gift that will fund a new pediatric residency.
