Human Obesity and the Role of the Physician Assistant
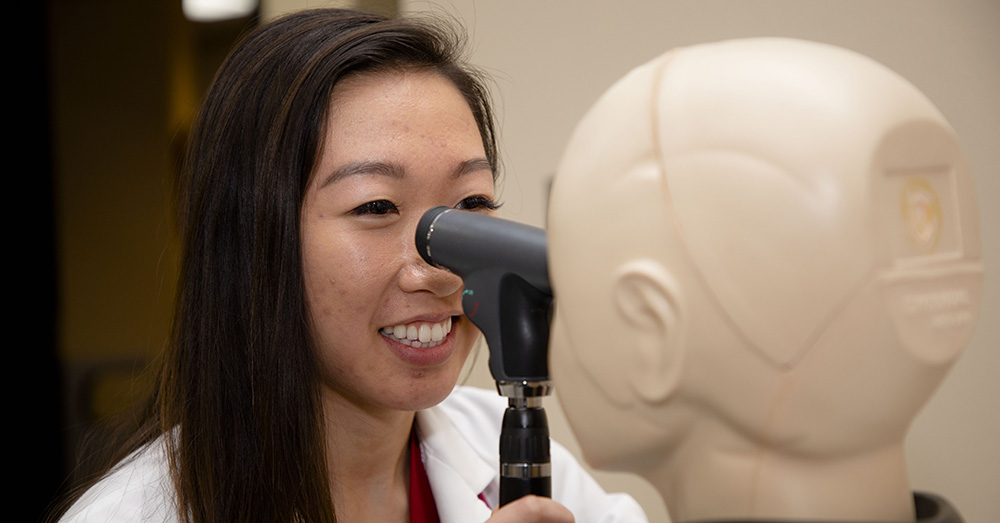
Diving into the neurobiological aspects of obesity and the ways physician assistants can fill the knowledge gap.

Obesity is a medical problem that can lead to or exacerbate other diseases and health problems including heart disease, diabetes, high blood pressure and some cancers. Rates of obesity in the United States have been rising steadily for years, and the ramifications are catastrophic.
We spoke with Dr. Chanaka N Kahathuduwa, M.B.B.S., M.Phil., Ph.D, an Assistant Professor in the Texas Tech University Health Sciences Center’s Physician Assistant Program, about the causes and effects of human obesity and how Physician Assistants (PAs) are equipped to diagnose and treat the problem.
The Obesity Pandemic

While often referred to as an epidemic, Kahathuduwa says that obesity is actually a pandemic, spreading across all continents of the world. “The rise is more prevalent in states with low socioeconomic statuses and states with less access to healthcare services,” he says. Obesity is more likely to cause complications in underserved communities.
The diagnosis of obesity is based on the body mass index criteria (BMI). In adults, a BMI over 30 kg/m2 equates to having obesity, but health complications can come into play earlier, at lower BMIs.
For children, Kahathuduwa points out that BMI must be considered compared to their age and sex.
“Childhood obesity is a rising problem,” he says. “The prevalence of childhood obesity is rising at a more marked rate than in adults.”
And sadly, obesity often goes undiagnosed until the patients present with a devastating complication.
“If someone doesn’t seek healthcare, they’re less likely to be diagnosed with obesity and more likely to remain unaware of the complications,” Kahathuduwa says. “And they don’t seek treatment.”
According to the Center for Disease Control and Prevention (CDC), the rates of obesity are continuing to rise with lower-capita states suffering the most.
“These are small towns without access to outlets of fresh produce such as farmer’s markets, the only food outlet available to some communities is a fast food restaurant” Kahathuduwa points out.
There are also fewer resources to get adequate physical activity. It’s easy to say, “Go to the gym,” but what if the town doesn’t have a gym or even a safe sidewalk?
Treating Obesity
When it comes to treating obesity, Kahathuduwa says there are many factors to consider. In cases of mildly increased BMI, a patient may benefit from behavioral management and counseling so they can work on their own to bring their weight down.
“They might be referred to a dietician, who may work with them to formulate a diet plan and may teach them important skills, such as how to count and restrict calories and how to correctly read and interpret a food label,” he says.
For some patients, controlling portion sizes works. For those who find this difficult, meal replacement solutions can help. Physical activity is also an important part of addressing obesity. Quoting one of his former supervisors, Dr. Nikhil Dhurandhar, Kahathuduwa says, “It’s important to remember that a patient doesn’t choose obesity, obesity chooses them.”
When portion control or meal replacement isn’t enough, there are more advanced treatment options including medication, weight control devices and bariatric surgery.
“There are about 10 FDA approved medications that work well in the short term,” Kahathuduwa says. “There are at least four commonly performed types of bariatric surgery.”
Kahathuduwa points out that medication and/or surgery tend to work in the short to medium term.
“Long term is hard to nail down,” he says.
All Roads Lead to the Brain
“Based on my research experience in neuroscience as related to obesity and ingestive behavior, the solution to obesity might be in the brain,” Kahathuduwa says. He explains that there are a lot of factors that contribute to obesity, but many of those contributors, especially the biological factors, converge in the brain.
“A lot of hormones are playing a role,” he says.
There are cognitive factors at play that must be understood and addressed. All of these things might be contributing, but they are not solely responsible.
“None of these are villains by themselves,” he says.
Lack of knowledge and lack of access to healthcare have contributed to this pandemic of obesity.
There are many factors that contribute to the problem, such as intake of excessive calories, for example as fast food or limited physical activity, but none of these can be blamed as ‘the’ single cause of obesity.
How Physicians Assistants Can Help Fight Obesity
“We have a limited number of physicians in the United States, especially in West Texas,” Kahathuduwa says. “The PA Profession and especially the TTUHSC PA program have been established with the mission of serving the underserved.”
With health care provider shortages, PAs can increase the efficiency and have proved to be a cost-effective way to improve health care. PAs are well equipped to provide comprehensive care and education to patients and assess risk factors to obesity and its complications. PAs can bridge the gap, especially in underserved and rural communities.
“They’re better able to fill the knowledge gap among patients,” Kahathuduwa says. “PAs are trained to do everything a doctor can do to manage and prevent obesity at the primary care level, especially in underserved communities.”
Through this, PAs can have a meaningful positive impact in the fight against the obesity pandemic.
Related Stories
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
Making Mental Health a Priority in the New Year
Sarah Mallard Wakefield, M.D., a psychiatrist with Texas Tech Physicians, talks about strategies to combat widespread and growing anxiety.
TTUHSC Dean to be Inducted into the National Academies of Practice as Distinguished Fellow
Gerard E. Carrino, Ph.D., MPH, dean of the TTUHSC Julia Jones Matthews School of Population and Public Health, will be inducted into the National Academies of Practice (NAP) as a Distinguished Fellow of the Public Health Academy.
Recent Stories
TTUHSC University Awards Ceremony Honors Recipients
On February 19, TTUHSC honored recipients at the University Awards, which held a significant change in 2026 by combining the annual recognition ceremonies for the first time.
National Academy of Inventors Names TTUHSC Faculty Senior Members
The National Academy of Inventors (NAI) has designated two current and one former TTUHSC faculty researchers as Senior Members.
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
