Relief and Hope for Those with Severe Depression

Dana Bear has suffered from severe depression her entire adult life. She has lived with suicidal tendencies, turned to alcohol to disguise her struggles and fought years of living with the symptoms of the disease.
“I started noticing my depression in my early adulthood,” Bear said. “At that point in time, I didn't do anything about it. It wasn't that bad until about 40 years ago and I have been working with it trying to get it under control since then. I basically have been on medication for around 30 years. It has worked some, but the depression always comes back, and my depression is severe in that I can really feel it and I also get suicidal.”
According to the National Institute of Mental Health, severe depression is one of
the most common mental disorders in the United States. Major depression impacts more
than 16.1 million
U.S. adults.
“I describe it a lot of times as thinking through mud, where everything just seems harder and everything seems heavy, but it's just very effortful throughout the day,” said Sarah Mallard Wakefield, M.D., chair of the Department of Psychiatry at the Texas Tech University Health Sciences Center School of Medicine. “You're exhausted trying to do even routine daily activities. The more severe the depression gets, the harder it is to function day to day, and some people find themselves not able to participate in activities of daily living because the weight is just too heavy.”
Bear said many think they know what depression is and then stigmatize people based on those beliefs. She wanted to be clear, depression is not a choice.
“I know lots of people think depressed people can't work or do anything,” Bear said. “But I have had to take care of myself and I had to work. I learned how to put on this mask and just fake it and that was pretty exhausting. This can affect people who are working 40 hours a week, if not more, and still putting on a brave face.”
Antidepressant medications are often the first treatment patients turn to, but for millions of Americans medications are not an effective solution. When patients have tried and failed several medications, health care professionals may recommend additional treatment options.
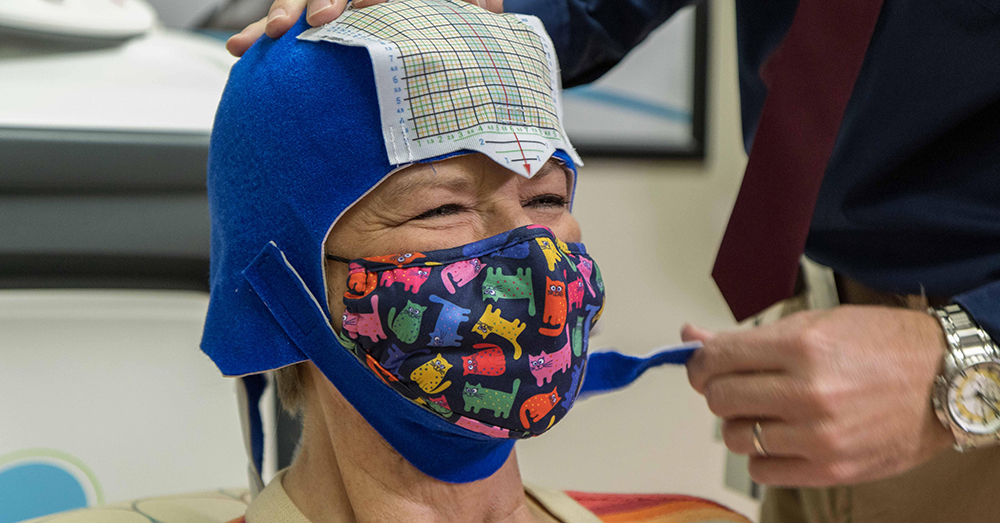
In her lifetime of depression, Bear has gone through counseling and therapies and has been prescribed many medications, some with side effects. Although she had a combination of treatments, Bear still suffered from the symptoms of depression. She spoke to Kenneth Ritchie, a physician assistant in the Department of Psychiatry, who suggested a treatment called transcranial magnetic stimulation (TMS).
TMS is a noninvasive procedure that uses magnetic fields to stimulate nerve cells
in the brain to improve symptoms of depression. The treatment for severe depression
involves delivering repetitive magnetic pulses to a specific area of the brain. TMS
is typically used when other depression treatments have not been effective.
The dorsolateral prefrontal cortex has connections to the limbic system, which is
involved in behavioral and emotional responses. Neuroimaging has shown decreased neuronal
activity in the dorsolateral prefrontal cortex of patients with depression.
“The brain is both a chemical and an electrical organ,” Wakefield said. “In a typical treatment of depression with medication, we are targeting increases in neurotransmitters, the chemicals in the brain. When we use TMS, electricity is being sent through a helmet or coil that is placed next to a patient's head to create a magnetic field. That magnetic field actually passes through the skull and induces an electric current that increases activity of neurons, thereby increasing neurotransmitters, or that chemical activity. We know that depression tends to show low neuronal activity in the dorsolateral prefrontal cortex. With TMS, we target that area to enhance that neuron signaling.”

With TMS, there are 36 sessions performed in total. The first 30 sessions are performed
five days a week, Monday through Friday, for six weeks. The last six sessions are
tapering sessions used to transition the frequency of visit from every day to every
few days. Each session lasts approximately 20 minutes. During each session, the helmet
or coil is placed on the patient’s head and the stimulation to the dorsolateral prefrontal
cortex is delivered in two-second pulses followed by a 20-second rest period. This
sequence repeats itself for approximately 20 minutes.
Patients report hearing clicking sounds and feeling a tapping on their forehead. Bear
said it does not hurt and is similar to the sounds of an MRI.
TMS is a very safe, non-invasive procedure. The most common side effect is having a headache after sessions at the beginning of treatment. TMS is FDA approved for those experiencing severe depression and who are 18 years of age and older.
Wakefield said TMS and antidepressants can actually complement each other well. Many
patients are on antidepressants when they begin TMS treatment. In these cases, physicians
do not stop their current medications and have had good results using both treatments
simultaneously.
“Many people benefit from TMS and do not need additional treatments in the future,”
Wakefield said. “There are people who benefit from staying on medication or starting
medication later, but they have better results from that treatment than they would
have otherwise because they engaged in TMS.”
Bear said after two weeks she began to feel positive results.
“I'm not saying everything has been perfect since,” Bear said. “I have had a day where I felt a little depression but it hasn't been anything near what I had felt before. I have good friends who have told me I sound so much better. People could tell in my voice that I felt better and that I was happier. I feel a little less heavy, you know, a little more helpful. When I left here my last time I was very, very happy with the results that I had gotten, because I had this feeling of being hopeful. I hadn't felt that in so long.”
Related Stories
Celebrating Veterans: TTUHSC’s General Martin Clay’s Legacy of Service and Leadership
From his initial enlistment in the Army National Guard 36 years ago to his leadership in military and civilian health care management roles, Major General Martin Clay’s career has been shaped by adaptability, mission focus and service to others.
Texas Tech University Health Sciences Center School of Nursing Named Best Accelerated Bachelor of Science in Nursing Program in Texas
The TTUHSC School of Nursing Accelerated Bachelor of Science in Nursing (BSN) program has been ranked the No. 1 accelerated nursing program in Texas by RegisteredNursing.org.
TTUHSC Names New Regional Dean for the School of Nursing
Louise Rice, DNP, RN, has been named regional dean of the TTUHSC School of Nursing on the Amarillo campus.
Recent Stories
TTUHSC University Awards Ceremony Honors Recipients
On February 19, TTUHSC honored recipients at the University Awards, which held a significant change in 2026 by combining the annual recognition ceremonies for the first time.
National Academy of Inventors Names TTUHSC Faculty Senior Members
The National Academy of Inventors (NAI) has designated two current and one former TTUHSC faculty researchers as Senior Members.
The John Wayne Cancer Foundation Surgical Oncology Fellowship Program at Texas Tech University Health Sciences Center Announced
TTUHSC is collaborating with the John Wayne Cancer Foundation and has established the Big Cure Endowment, which supports the university’s efforts to reduce cancer incidence and increase survivability of people in rural and underserved areas.
